Last Updated: December 5, 2024
Health Department Alert:

Last Updated: December 5, 2024
Mpox is a rare disease in the U.S. It is caused by the mpox virus, which belongs to the same group of viruses as smallpox. Mpox can make you sick including a rash or sores (pox), often with an earlier flu-like illness.
Mpox was previously called monkeypox. It was recently renamed following a World Health Organization decision.
Information about the current outbreak, including case numbers, is available from the Virginia Department of Health. Additional information is also available from the Centers for Disease Control and Prevention (CDC).
For additional information, visit VDH Mpox Basics.
![]() If you are sick and have symptoms consistent with mpox, seek medical care from your healthcare provider. Call ahead and let them know you are concerned about possible mpox infection so they can take precautions to ensure that others are not exposed.
If you are sick and have symptoms consistent with mpox, seek medical care from your healthcare provider. Call ahead and let them know you are concerned about possible mpox infection so they can take precautions to ensure that others are not exposed.
If you do not have a health care provider, please call 703-246-2433 for assistance.
The mpox virus is spreading mostly through close, intimate contact with someone who has mpox. The mpox virus can spread when a person comes into contact with the virus from a human, animal or from materials contaminated with the virus.
The risk is considered low for getting mpox by touching objects, fabrics, and surfaces that have been used by someone with mpox and not disinfected, such as clothing, bedding, towels, fetish gear, or sex toys.
Other ways the mpox virus can spread include:
Mpox does not spread from person to person through:
A person with mpox can spread it to others from the time symptoms start until the rash has fully healed and a fresh layer of skin has formed. As of February 2023, new data show that some people can spread mpox to others from one to four days before their symptoms appear. It’s not clear how many people this has affected during the current outbreak. There is currently no evidence showing that people who never develop symptoms have spread the virus to someone else.
Mpox symptoms usually start within 3 weeks of exposure to the virus. For most people, clear up within two to four weeks.
The illness often begins with:
You may experience all or only a few symptoms.
If someone has flu-like symptoms, they will usually develop a rash 1-4 days later. The rash can look like pimples or blisters. It often begins on the genitals or anus, or in and around the mouth. In these situations, the mpox rash could be confused with a more common sexually transmitted infection (STI). The rash might develop on just one part of the body or can appear on many parts of the body. These lesions might be painful.
People with certain conditions may be more likely to develop severe illness. These include people with weakened immune systems, children under 8 years of age, people with a history of eczema, and people who are pregnant or breastfeeding.
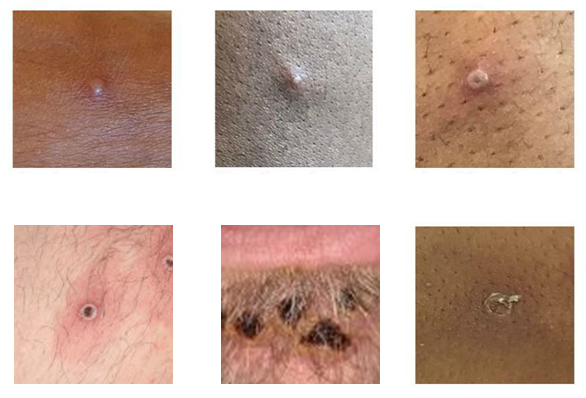
Photo credit: UK Health Security Agency, Source: CDC.
Take the following steps to prevent getting mpox:
While public health works to contain the current outbreak, we want you to have information so you can make informed choices when you are in spaces or situations where mpox could be spread. Mpox is often transmitted through close, sustained physical contact, almost exclusively associated with sexual contact in the current outbreak.
Vaccination is an important tool in preventing the spread of mpox. If you are at risk for mpox but haven’t received your two-dose vaccine yet, temporarily changing some parts of your sex life might reduce the risk of exposure to the virus. This includes the time between your first and second shots of vaccine. See below to learn more about vaccination.
See CDC's Social Gatherings, Safer Sex, and Mpox to learn more about:
Your healthcare provider may take a specimen and send it to a lab for testing or they may send you to a lab for both specimen collection and testing.
Learn more about testing from the CDC.
Please call ahead before going to a healthcare facility and let them know that you are concerned about mpox.
If you have mpox, you are advised to stay at home (isolate) until your mpox rash has healed and a new layer of skin has formed. Staying away from other people and not sharing things you have touched with others will help prevent the spread of mpox. Mpox can also spread to animals, so staying away from pets, livestock and other animals is important.
It’s important to notify your close contacts that they may have been exposed to mpox as soon as possible, so they can watch for signs and symptoms, get tested and isolate if they have symptoms, and consider getting vaccinated.
The Health Department can help you confidentially notify your contacts and help them monitor their symptoms so that if they do get sick, they can get tested quickly.
As with many viral illnesses, treatment mainly involves supportive care and relief of symptoms. Learn how to take care of yourself and manage your symptoms.
There are no treatments specifically for mpox virus infections. However, mpox and smallpox viruses are genetically similar, which means that antiviral drugs and vaccines developed to protect against smallpox may be used to prevent and treat mpox virus infections.
Antivirals, such as tecovirimat (TPOXX), may be recommended for people who are more likely to get severely ill, like patients with weakened immune systems. Not everyone who has symptoms of mpox is recommended to take treatments.
See Patient’s Guide to Mpox Treatment with Tecovirimat (TPOXX) from the CDC.
The CDC is closely monitoring worldwide case counts and working to understand the cause of the current cases.
Researchers are also investigating:
The first confirmed U.S. case in the outbreak was announced on May 18, 2022. The first case of Mpox in Northern Virginia was confirmed on May 27, 2022. Since that date additional cases have been identified in multiple states including in Virginia. On August 4, 2022, the U.S. Department of Health and Human Services declared a public health emergency in response to the mpox outbreak. The U.S. Public Health Emergency for mpox ended on January 31, 2023. However, mpox continues to be an important public health issue.
The Fairfax County Health Department is working with the Virginia Department of Health (VDH) and with other local public health agencies to respond to the current mpox outbreak. Key activities include:
The mpox vaccine is recommended for individuals who have been exposed, or are at high risk of exposure, to the virus.
Two vaccines may be used for the prevention of mpox disease:
At this time, JYNNEOS is the primary vaccine used in Virginia for prevention of mpox.
People can be vaccinated after exposure to mpox virus to help prevent mpox. This is called "post-exposure prophylaxis."
People should take precautions to reduce their exposure to mpox until two weeks after receiving the second vaccine dose and immune protection from vaccines has reached its maximum.
The mpox vaccine is recommended for individuals who have been exposed, or are at high risk of exposure to the mpox virus.
VDH updated its vaccine eligibility in February 2023. VDH and CDC recommends vaccination against mpox if you:
At this time, most clinicians and laboratorians in the United States are not advised to receive mpox vaccine pre-exposure prophylaxis (PrEP).
Non-residents of Virginia are now eligible to receive the JYNNEOS mpox vaccine.
An FDA emergency authorization enables a change in how the currently licensed JYNNEOS vaccine is administered. Research shows that giving the JYNNEOS vaccine intradermally is safe and causes a similar immune response against mpox while using a smaller dose. This will enable more people to be vaccinated better protecting our community.
On August 24, the health department began vaccinating individuals 18 years and older who are eligible for the JYNNEOS vaccine with an intradermal injection - a shot given between the layers of the skin (like a TB test), rather than below the skin (subcutaneous). Note: If you have a history of developing keloids, tell your provider. They may suggest getting the vaccine subcutaneously instead.
Two doses of the vaccine are needed. People who received their first dose as a subcutaneous injection can get their second dose intradermally.
Learn more about how the vaccine is given intradermally and possible side effects from this VDH factsheet.
For more information, see:
You should still continue to take precautions after vaccination.
The JYNNEOS vaccine is given in two-doses with 28 days between doses. You are considered protected 14 days after your second dose (about 6 weeks after your first dose). You should continue to take precautions against mpox between doses.
Mpox infections after vaccination are possible, although they may be milder and less likely to result in hospitalization. You can reduce your risk of infection by continuing to take preventative measures after being vaccinated. CDC offers more information about mpox infections after vaccination.
For more information about mpox vaccines and other prevention measures, please visit the CDC Prevention website.
The Virginia Department of Health provides information about mpox for healthcare professionals, including those working in acute care hospitals, physicians’ offices, urgent care centers, and outpatient clinics. The recommendations and guidance may also be applicable to other settings where health care is delivered, such as school/work health clinics.
If evaluating a patient suspected to have mpox, call your local health department and implement appropriate infection prevention precautions.
Additional information for clinicians is available from the CDC.
