Please wait while we redirect you to the right page...
Archived page: This page is no longer being updated and is available as a reference only.
If you need a vaccine, find out how to make an appointment.

Please wait while we redirect you to the right page...
Archived page: This page is no longer being updated and is available as a reference only.
If you need a vaccine, find out how to make an appointment.
See our new partner portal for local community leaders and organizations with shareable information about COVID-19 safety curated according to health messages.
Find health alerts, guidance for patients, and other information for Health Care Providers
Additional resources from Fairfax County are available on the COVID-19 Language Portal.
A full list of materials available on our resources page.
While many are staying at home during the pandemic, people who live in apartments or condos should consider additional steps they can take to limit the spread of the COVID-19. Property owners also can take extra precautions to help keep their residents safe. See the recommendations.
See also: Households Living in Close Quarters | Living in Shared Housing | Handout
The Health Department offers the following guidance for Community-Based Organizations to enhance the safety of your staff and volunteers and reduce their risk of COVID-19 infection, as well as providing guidance on how the risk of potential transmission to clients can be reduced.
The following lists recommendations for service providers and the rationales for those recommendations. The CDC also has extensive guidance for providers that highlights additional situations and issues for consideration.
Additionally, two checklists are available for download to help your organization plan:
If you have additional questions, please email ffxcovid@fairfaxcounty.gov.
Find COVID-19 and other resources from the Virginia Department of Health. Find resources.
The CDC has several videos available in American Sign Language. See the playlist.
See the COVID-19 Updates for Food Establishments page for the latest guidelines.
Helpful Tips and Information for Food Establishments Poster
Shopping for Food During the COVID-19 Pandemic - Information for Consumers
This information provides current resources or information specifically for businesses.
Returning To Work: Employers should not require employees to provide a negative COVID-19 test result or a healthcare provider’s note to enable them to return to work. An employee can return to work once certain situations are met. Learn more about what employers should know.
Watch: Fairfax County Businesses Adapt During the Pandemic
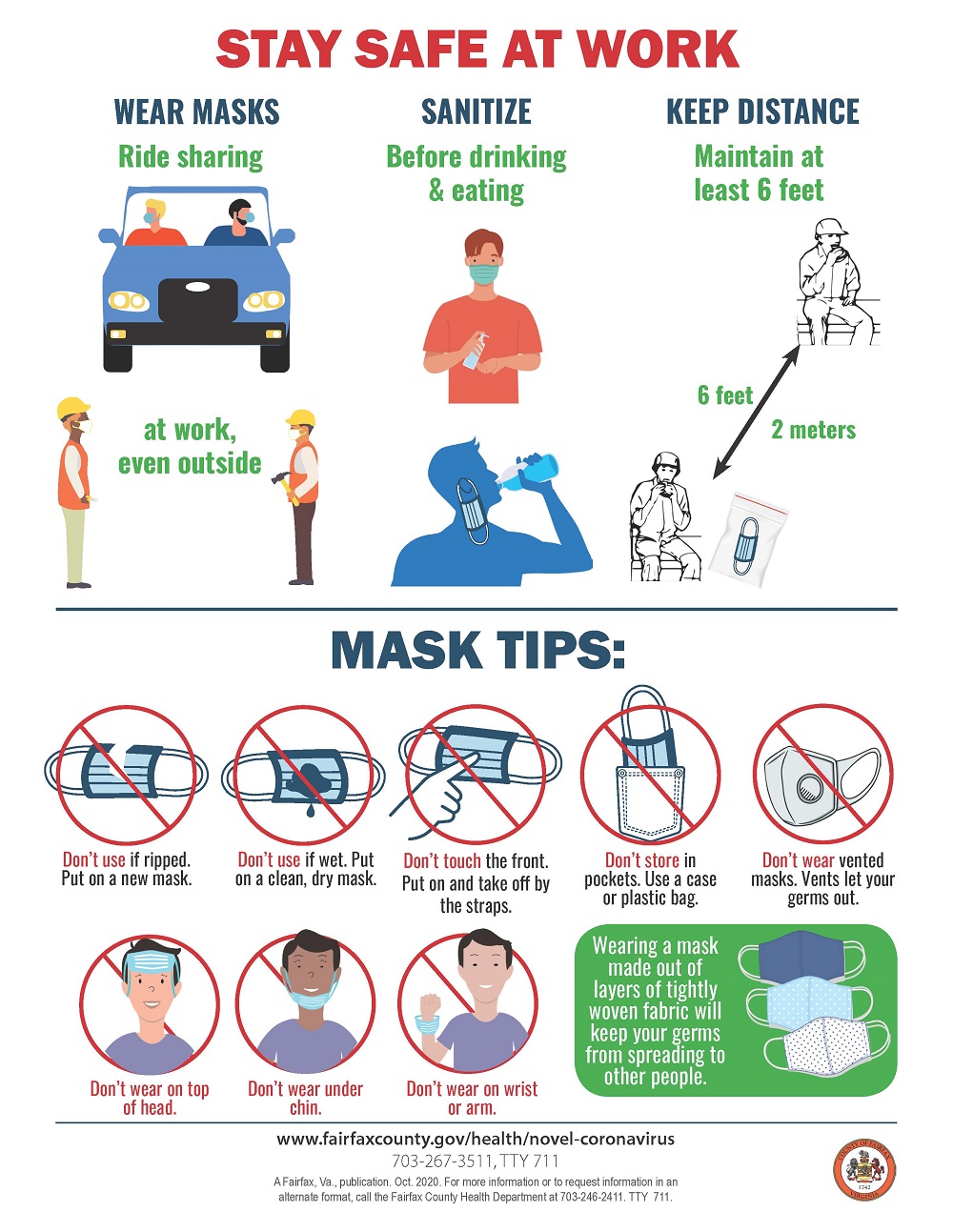
Infographics:
The Health Department is working to prevent and mitigate outbreaks in long-term care facilities. Please see: COVID-19 Prevention and Mitigation for Long-Term Care Facilities.
While fewer children have been sick with COVID-19 compared to adults, children can be infected with the virus that causes COVID-19, can get sick from COVID-19, and can spread the virus that causes COVID-19 to others.
While most reported cases in children are either asymptomatic or mild, there have been cases of severe illness and some children do need to be hospitalized. In spring 2020, doctors recognized a severe syndrome in children, many of whom had evidence of recent COVID-19 infection. multisystem inflammatory syndrome (MIS-C).
Fairfax County Public Schools has developed information for talking to children about coronavirus.
The CDC also offers information for Children and Teens.
VDH has Guidance for College Students on College Campuses.
For school district- specific information, please visit:
FCPS offers grab and go food distribution sites, including pop-up sites in the community, curbside pickup at two schools, and meal delivery along some bus routes. Details on locations and times is available here.
Among adults, the risk for severe illness from COVID-19 increases with age, with older adults at highest risk. Severe illness means that the person with COVID-19 may require hospitalization, intensive care, or a ventilator to help them breathe, or they may even die. See more information for Older Adults from the CDC.
We are learning more about COVID-19 every day. The below list of underlying medical conditions is not exhaustive and only includes conditions with sufficient evidence to draw conclusions; it is a living document that may be updated at any time, subject to potentially rapid change as the science evolves. For the latest information, please visit CDC's People with Certain Medical Conditions page.
Adults of any age with the following conditions are at increased risk of severe illness from COVID-19:
COVID-19 is a new disease. Currently there are limited data and information about the impact of underlying medical conditions and whether they increase the risk for severe illness from COVID-19. Based on what we know at this time, people with the following conditions might be at an increased risk for severe illness from COVID-19:
Many travelers are concerned about the current COVID-19 pandemic and may be wondering how to travel safely, or if it’s a good idea to go at all. Airports, bus stations, train stations, and rest stops are all places travelers can be exposed to the virus, both in the air and on surfaces. These are also places where it can be hard to social distance. Learn more about steps to take before and after traveling.
Staying home is the best way to protect yourself and others from COVID-19, but there are times when travel may be unavoidable. Because each of us plays a part in slowing the spread of COVID-19, follow these Centers for Disease Control and Prevention (CDC) recommendations before, during and after your trip.
CDC's Websites:
VDH’s website: Virginia Travelers have questions.
CDC recommends that all people defer travel on cruise ships, including river cruises, worldwide. See the Level 3 Travel Advisory and Guidance for Travelers Returning from Cruise Ship and River Cruise Voyages.
On April 9, 2020, CDC renewed the No Sail Order and Other Measures Related to Operations Order. See Cruise Ship Guidance.
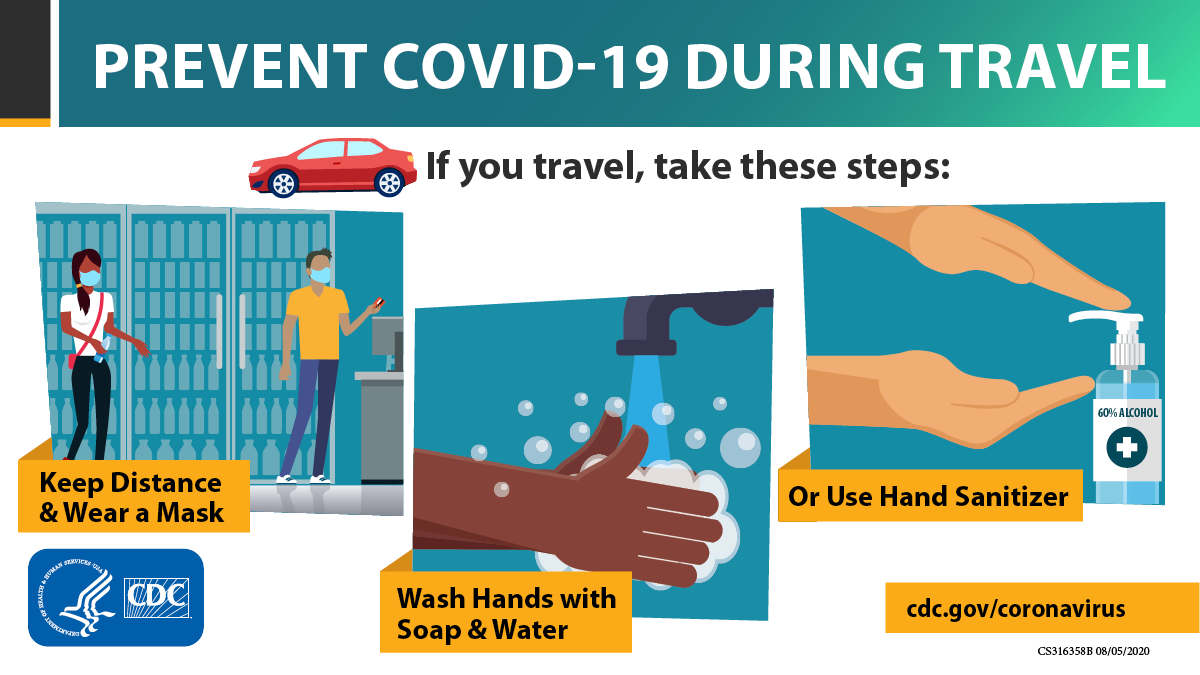
Infographics:
Find worker safety information from the CDC, including:
Employees: How to Cope with Job Stress and Build Resilience During the COVID-19 Pandemic
What Construction Workers Need to Know about COVID-19
What Food and Grocery Pick-up and Delivery Drivers Need to Know about COVID-19
What Grocery and Food Retail Workers Need to Know about COVID-19
What Mail and Parcel Delivery Drivers Need to Know about COVID-19
What Rideshare, Taxi, Limo, and other Passenger Drivers-for-Hire Need to Know about COVID-19
