Definitions
Health Care Settings – Places where health care is delivered and includes, but is not limited to, acute care facilities, long-term acute-care facilities, nursing homes, home health care, vehicles.
Health Care Personnel (HCP) – All paid and unpaid persons serving in health care settings who have the potential for direct or indirect exposure to patients or infectious materials, including body substances.
Health Care Services – Includes hospice care, physical therapy, wound care, urinary catheter care, intravenous injections and any other procedures requiring licensed health care personnel.
Non-skilled Personal Care – Includes bathing, dressing, toileting, transferring, bowel control, bladder control and eating/feeding.
Source Control – The use of respirators, well-fitting masks, or well-fitting cloth masks to cover a person’s mouth and nose to prevent the spread of respiratory secretions when they are breathing, talking, sneezing, or coughing.
Up to Date – When a person has received all COVID-19 vaccines recommended to them by the CDC. See the COVID-19 Vaccines page.


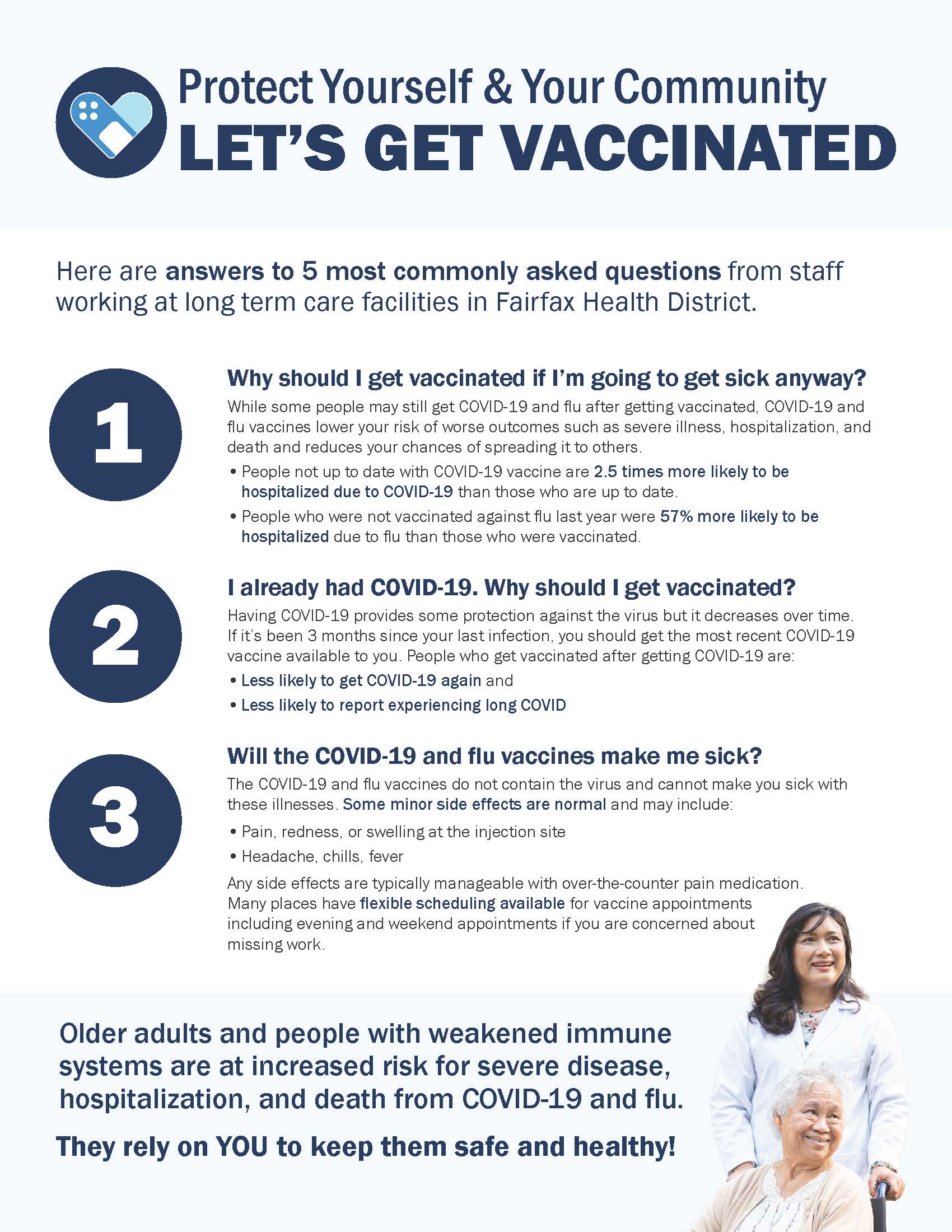 Older adults and people with weakened immune systems are at increased risk for severe disease, hospitalization, and death from COVID-19 and flu. They rely on YOU to keep them safe and healthy! See answers to the most commonly asked questions from staff working at long term care facilities in Fairfax Health District.
Older adults and people with weakened immune systems are at increased risk for severe disease, hospitalization, and death from COVID-19 and flu. They rely on YOU to keep them safe and healthy! See answers to the most commonly asked questions from staff working at long term care facilities in Fairfax Health District.