Mpox symptoms usually start within 3 weeks of exposure to the virus. For most people, clear up within two to four weeks.
The illness often begins with:
- Fever
- Headache
- Muscle aches
- Backache
- Swollen lymph nodes
- Chills
- Exhaustion
- Respiratory symptoms (e.g. sore throat, nasal congestion, or cough)
- A rash that may be located on or near the genitals or anus but could also be on other areas like the hands, feet, chest, face, or mouth.
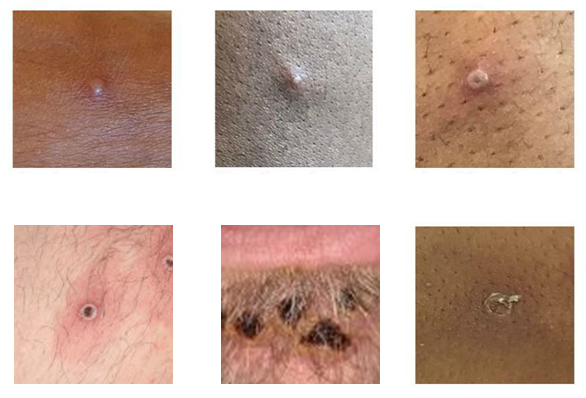
- The rash will go through several stages, including scabs, before healing.
- The rash can look like pimples or blisters and may be painful or itchy.
You may experience all or only a few symptoms.
- Sometimes, people have flu-like symptoms before the rash.
- Some people get a rash first, followed by other symptoms.
- Others only experience a rash.
If someone has flu-like symptoms, they will usually develop a rash 1-4 days later. The rash can look like pimples or blisters. It often begins on the genitals or anus, or in and around the mouth. In these situations, the mpox rash could be confused with a more common sexually transmitted infection (STI). The rash might develop on just one part of the body or can appear on many parts of the body. These lesions might be painful.
People with certain conditions may be more likely to develop severe illness. These include people with weakened immune systems, children under 8 years of age, people with a history of eczema, and people who are pregnant or breastfeeding.
If you have symptoms, separate yourself from other people and pets, cover your lesions, and contact your healthcare provider, even if you don’t think you had contact with someone who has mpox.
Mpox Rash Photos
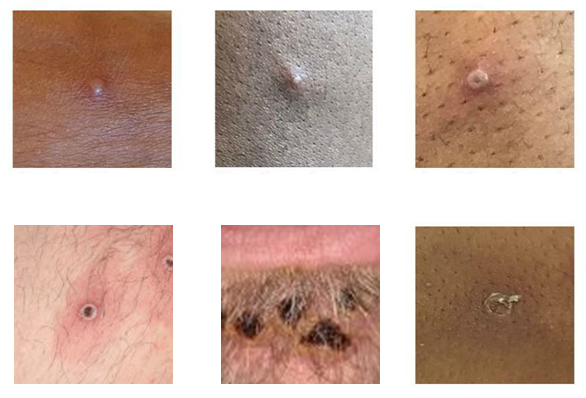
Photo credit: UK Health Security Agency, Source: CDC.